Featured Articles

Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
A Brief History of Gout
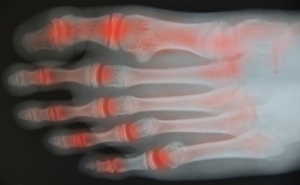
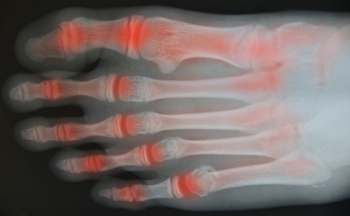
Gout is a type of arthritis which causes uric acid crystals to form on joints—most commonly in the big toe. Symptoms may include pain, inflammation, redness, and limited range of motion. Gout was first identified around 2640 B.C. in ancient Egypt, and has been studied by countless scientists and physicians dating back to Hippocrates who called it “the unwalkable disease”. Uric acid crystals from a gouty deposit were first seen under a microscope in 1679, and the 19th century chemist, Emil Fischer’s, work established the relationship between uric acid and purine—which can raise levels of uric acid in the body. Some famous people who may have experienced gout include King Henry III, Sir Issac Newton, Ben Franklin, Sir Lawrence Olivier, David Wells, Jim Belushi, and Jared Leto—after gaining 60 lbs. for a movie role. Risk factors include eating a diet high in purines, a family history of gout, obesity, certain medical conditions and medications, and more. If you have pain or inflammation in your big toe, make an appointment with a podiatrist for an examination.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Everything You Need to Know About Gout
Gout, typically found in diabetic patients, is an unusually painful form of arthritis caused by elevated levels of uric acid in the bloodstream. The condition typically strikes the big joint on the big toe. It has also been known to strike the knees, elbows, fingers, ankles and wrists—generally anywhere that has a functioning, moving joint.
The high level of uric acid in a person’s bloodstream creates the condition known as hyperuricema—the main cause of gout. Genetic predisposition occurs in nine out of ten sufferers. The children of parents who suffer gout will have a two in ten chance of developing the condition as well.
This form of arthritis, being particularly painful, is the leftover uric acid crystallizing in the blood stream. The crystallized uric acid then travels to the space between joints where they rub, causing friction when the patient moves. Symptoms include: pain, redness, swelling, and inflammation. Additional side effects may include fatigue and fever, although reports of these effects are very rare. Some patients have reported that pain may intensify when the temperature drops, such as when you sleep.
Most cases of gout are easily diagnosed by a podiatrist’s assessment of the various symptoms. Defined tests can also be performed. A blood test to detect elevated levels of uric acid is often used as well as an x-ray to diagnose visible and chronic gout.
Treatment for gout simply means eliminating symptoms. Non-steroid anti-inflammatory drugs or NSAIDs (Colchicine and other corticosteroid drugs, etc.) will quell the redness, the swelling, and the inflammation. However, managing your diet, lifestyle changes, and using preventative drugs are all helpful toward fully combating the most severe cases.
Those that lead an inactive lifestyle are at a higher risk for gout. Any amount of exercise decreases the probability of repeat encounters with the condition. Reducing your consumption of red meat, sea food, and fructose-sweetened drinks also reduces the likelihood of chronic gout as well.
Ingesting Vitamin C, coffee, and particular dairy products can help with maintaining a healthy lifestyle. There are new drugs out on the market that inhibit the body’s production of uric acid-producing enzymes. However, reducing or eliminating your overall levels of uric acid is the best remedy to ensuring you lead a gout-free life.
Caring for Aging Feet
 As the feet age, they begin to experience more wear and tear. The joints in the feet become stressed, and the skin becomes thinner and less elastic. Signs of aging feet include aches and pains, development of bunions, circulatory issues and the toes beginning to curl up. Because foot issues can be debilitating, older patients should take care of their feet. Common things that can be done to help reduce the effects of aging include exercise, general foot care (proper toenail trimming, checking for problems to detect them early, and moisturizing the feet), and wearing properly fitting shoes. Another key to help with aging feet is having an annual check with a podiatrist. Visiting a podiatrist can help find issues such as diabetes or poor circulation, and podiatrists can help treat common foot problems like bunions, ingrown toenails, and cracked heels.
As the feet age, they begin to experience more wear and tear. The joints in the feet become stressed, and the skin becomes thinner and less elastic. Signs of aging feet include aches and pains, development of bunions, circulatory issues and the toes beginning to curl up. Because foot issues can be debilitating, older patients should take care of their feet. Common things that can be done to help reduce the effects of aging include exercise, general foot care (proper toenail trimming, checking for problems to detect them early, and moisturizing the feet), and wearing properly fitting shoes. Another key to help with aging feet is having an annual check with a podiatrist. Visiting a podiatrist can help find issues such as diabetes or poor circulation, and podiatrists can help treat common foot problems like bunions, ingrown toenails, and cracked heels.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Taking Care of Elderly Feet
Many foot diseases and conditions become more serious and common among the elderly. Some of these conditions include diabetic ulcers, ingrown toenails, fungus, arthritis, corns, and calluses. Unfortunately, it may be harder for older adults to take care of their own feet, but there are some precautions they can take in order to avoid any serious conditions.
Dry, cracked heels tend to be a common problem for older people. In order to avoid this, you should always keep your feet clean and well moisturized. Special feet moisturizers should be used as average lotions might not provide enough moisture for dry and cracked heels. Daily foot inspections are crucial for the elderly to detect any irregularities in their earliest stages. During the aging process, blood circulation tends to slow down causing older people to not feel their feet as well as they used to. This often results in foot problems going unnoticed.
Fungal and bacterial conditions thrive on elderly feet because older adults are less likely to keep their feet clean and dry; this makes it easier for bacteria to take hold in their dry, cracked skin. Elderly people should be sure to thoroughly dry their feet, especially in between the toes, after bathing. This will help them avoid developing any fungal infections. Additionally, clean cotton socks should be worn after the feet are dried.
Cutting toenails straight across will help prevent ingrown toenails. When toenails are cut too lose, the nail might break through the skin resulting in an ingrown nail. Clippers should be used to cut the nails in order to make the cut even.
Elderly people who have diabetes are at risk of developing serious foot problems that may lead to amputation. Ulcers that are left untreated can lead to gangrene. Dry and cracked feet, fungus, and untended cuts under the nails may also lead to infections.
Fortunately, Medicare covers many different types of services for foot care. Elderly people with any of these foot conditions should seek the help of a podiatrist and perform daily foot inspections in order to ensure that they have healthy feet.
Arthritis and the Big Toe
 Osteoarthritis, the type of arthritis that is associated with aging, can affect any joints in the body, including the big toe joint. As we age, the cartilage that lines joints breaks down due to wear and tear, causing symptoms such as swelling, pain, and stiffness in the affected joints. Osteoarthritis in the big toe can cause tenderness, achiness, and joint pain in the toe in its initial stages. As the arthritis progresses, you may also begin to feel burning or nerve pain in the toe. The symptoms are typically present at rest, and particularly after long periods of sitting or inactivity. Arthritis can also lead to excess bone growth in the big toe, causing the joint to fuse and become immobile. If you have symptoms of arthritis in your toes, please see a podiatrist for treatment.
Osteoarthritis, the type of arthritis that is associated with aging, can affect any joints in the body, including the big toe joint. As we age, the cartilage that lines joints breaks down due to wear and tear, causing symptoms such as swelling, pain, and stiffness in the affected joints. Osteoarthritis in the big toe can cause tenderness, achiness, and joint pain in the toe in its initial stages. As the arthritis progresses, you may also begin to feel burning or nerve pain in the toe. The symptoms are typically present at rest, and particularly after long periods of sitting or inactivity. Arthritis can also lead to excess bone growth in the big toe, causing the joint to fuse and become immobile. If you have symptoms of arthritis in your toes, please see a podiatrist for treatment.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
When Should I See a Doctor for Foot Warts?
 Warts that grow on the soles of feet are known as plantar warts. These fleshy, grainy patches of raised skin are known for their characteristic tiny, black dots that appear at their centers. Plantar warts are caused by the contagious human papillomavirus (HPV) entering the feet through a crack in the skin. Unlike other types of warts, plantar warts grow inwards, which can make walking uncomfortable. Warts on the feet generally respond well to treatment. If you have plantar warts that are causing you pain or discomfort, are discolored, show signs of infection such as bleeding, scabbing, and pus drainage, or if you have diabetes or an immune deficiency, you should see a podiatrist who can treat the warts and teach you how to prevent recurrences.
Warts that grow on the soles of feet are known as plantar warts. These fleshy, grainy patches of raised skin are known for their characteristic tiny, black dots that appear at their centers. Plantar warts are caused by the contagious human papillomavirus (HPV) entering the feet through a crack in the skin. Unlike other types of warts, plantar warts grow inwards, which can make walking uncomfortable. Warts on the feet generally respond well to treatment. If you have plantar warts that are causing you pain or discomfort, are discolored, show signs of infection such as bleeding, scabbing, and pus drainage, or if you have diabetes or an immune deficiency, you should see a podiatrist who can treat the warts and teach you how to prevent recurrences.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts
Plantar warts are growths that typically appear on the heels or other weight-bearing areas of the feet. These warts are caused by the human papillomavirus (HPV). The virus enters the body through breaks in the skin, such as cuts, that are on the bottom of the feet. Plantar warts are more likely to affect children and teenagers, people with weakened immune systems, people who have a history with plantar warts, and people who walk barefoot in environments exposed to a wart-causing virus.
If you suspect you have plantar warts, you may have the following symptoms: pain or tenderness while walking, a lesion that interrupts the ridges in the skin of your foot, small fleshy lesions on the bottom of the foot, or a callus where a wart has grown inward over a well-defined spot on the skin.
HPV causes plantar warts to form and is very common. There are more than 100 kinds of the virus in existence. However, only a few of them cause warts on the feet. The other types of HPV are likely to cause warts on other parts of the body.
If you have plantar warts, your podiatrist may try different treatment methods depending on your specific case. Some treatments for plantar warts are peeling medicines (salicylic acid), freezing medicines (cryotherapy), or surgical procedures. Laser treatments and vaccines are also used to treat plantar warts.