Featured Articles

Why Live with Pain and Numbness in Your Feet?
Causes and Risks of Ankle Sprains in Athletes

Ankle sprains are common injuries, with half occurring during athletic activities. This injury happens when the ligaments that support the ankle stretch or tear, often due to sudden twisting or rolling of the foot. Athletes are particularly susceptible during sports that involve jumping, running, or rapid direction changes. The ligaments most frequently affected are the anterior talofibular ligament, the calcaneofibular ligament, and the posterior talofibular ligament. These ligaments connect the bones of the ankle and provide stability to the joint. When they are injured, symptoms include pain, swelling, and difficulty walking. Proper diagnosis and treatment are essential for recovery, often involving rest, compression, and elevation. Preventative measures include proper footwear, strength training, and exercises to reduce the risk of future sprains. If you have sprained your ankle, it is suggested that you make an appointment with a podiatrist who can properly treat this condition.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
Definition and Types of Corns

Corns are thickened areas of skin that develop due to repeated friction or pressure, often on the feet. They typically form on the tops or sides of toes and can be painful when pressed. There are two main types of corns which are hard and soft. Hard corns are the most common, appearing as small, dense, and circular areas of thickened skin, usually found on the tops of toes or other bony areas. Soft corns, in contrast, are whitish and rubbery in texture, typically developing between the toes where the skin is moist from sweat. Both types of corns result from excessive pressure and friction, often due to wearing ill-fitting shoes or abnormal toe movements. Corns on the feet can be painful and may cause difficulty in completing daily tasks. If you have developed a corn, it is suggested that you speak to a podiatrist who can offer you effective relief options.
If you have any concerns regarding your feet and ankles, contact one of our podiatrists of Romeo Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctors to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
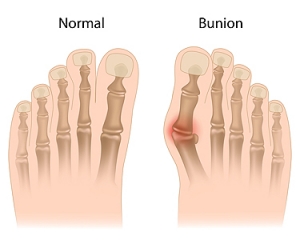
Understanding and Preventing Bunions
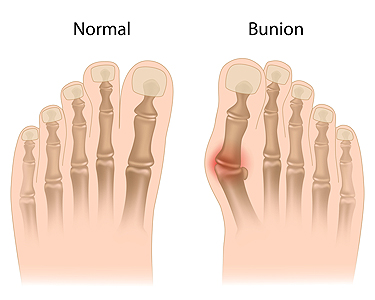
A bunion is a bony bump that forms at the base of the big toe, resulting from misalignment of the joint. It can cause pain, swelling, and difficulty in finding comfortable footwear. Genetics, wearing tight or ill-fitting shoes, and certain foot shapes can contribute to bunion development. To prevent bunions, it is important to wear shoes with a wide toe box and avoid high heels that put pressure on the front of the foot. Custom orthotics can provide support and alleviate pressure on the big toe joint. Stretching and strengthening exercises for the feet can improve alignment and reduce strain. Early intervention, such as using bunion pads and maintaining a healthy weight, can also help prevent the progression of bunions. If you have a bunion, it is suggested that you speak to a podiatrist who can provide you with additional methods for relief and treatment options.
If you are suffering from bunion pain, contact one of our podiatrists of Romeo Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Symptoms and Causes of Plantar Fasciitis

Foot pain can significantly disrupt daily activities and diminish quality of life, and plantar fasciitis is one of the main culprits. The plantar fascia is a thick band of tissue that stretches from the heel to the toes, supporting the foot’s arch and helping with movement. When this tissue becomes inflamed, it results in plantar fasciitis. This causes sharp heel pain that is especially noticeable with the first steps in the morning or after long periods of inactivity. Common causes of plantar fasciitis include biomechanical issues like flat feet or high arches, and overuse from activities such as running. Wearing shoes that lack proper support, tight calf muscles, and additional stress from excess body weight are other causes. Managing plantar fasciitis typically involves stretching exercises to relieve tension, wearing supportive footwear, and using orthotic inserts. Preventive measures focus on proper footwear and maintaining flexibility in the lower legs through regular stretching. If you are suffering from persistent heel pain, it’s suggested that you schedule an appointment with a podiatrist for an exam and suggestions for treatment, which can begin your journey to recovery and improved foot health.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Safeguarding Diabetic Limbs

Preventing amputation of diabetic limbs is essential in preserving mobility and enhancing the quality of life for individuals with diabetes. Regular foot care plays a pivotal role in this endeavor. Daily inspection of the feet for cuts, blisters, or ulcers, along with proper hygiene and moisturization, helps detect issues early and prevent complications. Choosing appropriate footwear that fits well and provides adequate support reduces the risk of pressure points and injuries. Managing blood sugar levels through diet, exercise, and medication adherence is critical in preventing nerve damage and promoting wound healing. Seeking prompt medical attention for any foot problems, no matter how minor, is essential to prevent them from escalating into more serious issues. Regular check-ups with podiatrists allow for comprehensive monitoring of foot health and early intervention if problems arise. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can discuss important measures for limb protection.
Diabetic Limb Salvage
Diabetic limb salvage can be an effective way in preventing the need for limb amputation. If you have a foot ulcer and diabetes, consult with one of our podiatrists from Romeo Foot & Ankle Clinic. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Diabetic Limb Salvage?
Diabetic limb salvage is the attempt of saving a limb, such as the foot, that has an infected ulcer, from amputation. Podiatrists also try to make sure that there is enough function in the foot after the salvage that it is still usable. Those with diabetes experience poor blood circulation, which prevents proper healing of an ulcer. If the ulcer is left uncheck, it could become infected, which could result in the need for amputation.
Diabetes is the number one cause of non-traumatic amputations in the United States. Amputation has been found to lead to higher mortality rates. This translates into higher healthcare costs, and a reduced quality of life and mobility for amputees. Podiatrists have attempted to increase the prevalence of limb salvage in an attempt to solve these issues.
Diagnosis and Treatment
Limb salvage teams have grown in recent years that utilize a number of different treatments to save the infected limb. This includes podiatrists that specialize in wound care, rehabilitation, orthotics, and surgery. Through a combination of these methods, limb salvage has been found to be an effective treatment for infected limbs, and as an alternative to amputation. Podiatrists will first evaluate the potential for limb salvage and determine if the limb can be saved or must be amputated.
If you have any questions, please feel free to contact our offices located in Washington and Shelby Townships, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.